High blood pressure, or hypertension, is a stealthy health condition affecting millions globally.
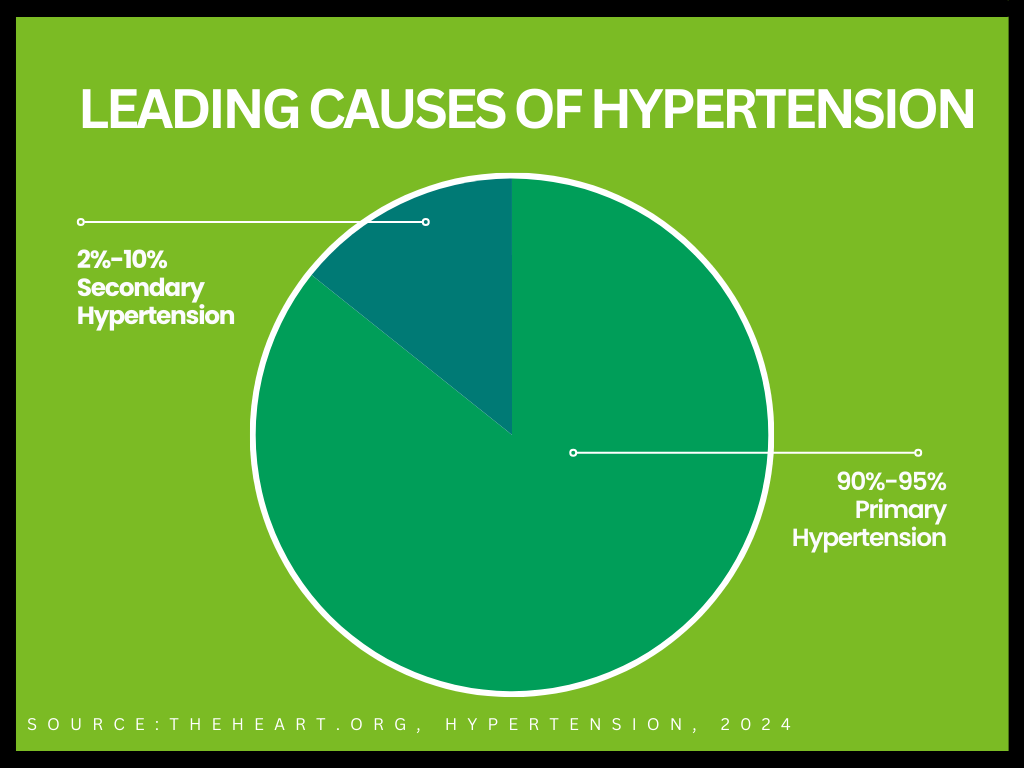
Hypertension comes in two main types: primary, which is also called essential hypertension, and secondary. For adults, primary hypertension is the type most often diagnosed.
Among the various causes, genetics or family history ranks as one of common contributors to hypertension.
Blood pressure is influenced by genetics, with studies showing that 30–50% of its variation can be inherited. Often going undetected due to its subtle onset, hypertension is a critical health issue that demands attention.
Hypertension: A Global Health Concern
Hypertension is a problem that affects everyone, no matter who they are, and it’s a big concern for health worldwide. It’s important to understand how high blood pressure works to manage and prevent it effectively.
This condition is often stealthy, presenting no specific symptoms but posing serious risks to cardiovascular health.
It’s defined by two measurements: systolic pressure, which occurs as the heart pumps blood, and diastolic pressure, when the heart is at rest. Normal pressure levels hover around 120/80 mmHg, with consistent readings above 130/80 mmHg considered hypertensive.
Want to learn more about hypertension? Check out the link below
Related Content: Everything You Need to Know About High Blood Pressure (Hypertension)
The Role of Genetics in Hypertension
Hypertension develops through a mix of genetics and how we live. Genetics play a big part in the risk of getting high blood pressure, so it’s important to consider this in its management.
Genetic Predisposition
Genetics play a crucial role in an individual’s susceptibility to hypertension.
Specific genes, such as those in the renin-angiotensin-aldosterone system (RAAS), which regulates blood pressure and fluid balance, have been identified as influential in the development of hypertension.
Family History
A family history of hypertension substantially raises an individual’s risk, underlining the importance of understanding familial health patterns.
Research on Genetic Markers
Ongoing research has identified several genetic markers linked to hypertension. For instance, variations in the genes like AGT, which is involved in blood vessel constriction, and CYP11B2, which affects salt retention, can increase hypertension risk.
| Quick Fact |
| AGT is a gene that helps control your blood pressure by making a protein that narrows blood vessels, which can increase blood pressure. CYP11B2 is another gene that makes a protein involved in controlling blood pressure, but it does so by managing the balance of salt and water in your body. Both of these genes are important because they work in your body’s system for keeping blood pressure just right. If they’re not working properly, it could lead to high blood pressure. |
Age and Ethnicity
The risk of developing high blood pressure increases with age. Additionally, hypertension prevalence and severity can differ among ethnic groups.
For instance, African Americans tend to develop hypertension at a younger age and often have more severe cases compared to other ethnic groups. In contrast, Caucasian and Hispanic populations have comparatively lower risks of early onset and severe hypertension.
Take a look at this bar chart—it breaks down the ages when adults from different racial and ethnic backgrounds — like Asian, White, Hispanic, and Black communities — first get diagnosed with hypertension.
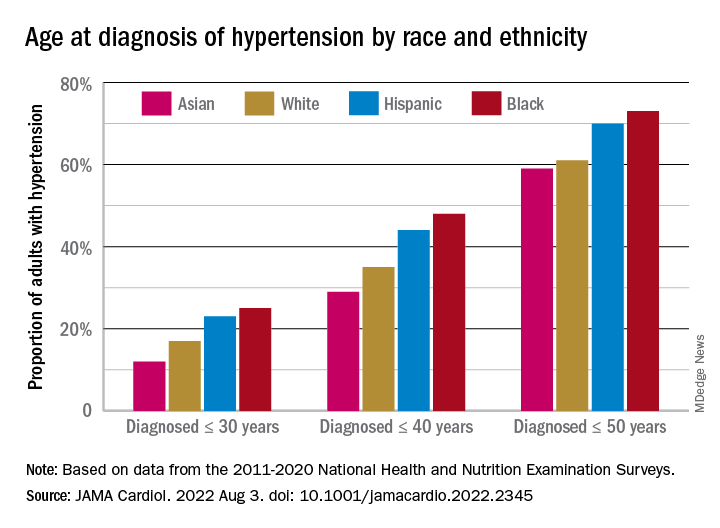
You can see the percentages for diagnoses made by age 30, 40, and up to 50. What this chart really puts into perspective is how the age of hypertension diagnosis isn’t the same across the board—it varies widely among these groups.
Hypertension Genetic Risk Assessment Checklist
Assess your genetic risk for hypertension by going through each item in this checklist. For each statement that applies to you, assign the corresponding points. At the end, tally up your total points to understand your potential risk level.
Disclaimer: This checklist is a general guide and not a definitive diagnostic tool. Always consult healthcare professionals for personalized health assessments and advice.
Family History Evaluation
- Family Member with Hypertension (5 points): Assign points if immediate family members (parents, siblings, grandparents) have or had hypertension. This factor increases your genetic predisposition.
- Early Onset in Family Members (10 points): Add points if hypertension was diagnosed in family members before age 55 for men and 65 for women, as early onset can indicate a stronger genetic link.
- Family History of Heart Disease or Stroke (5 points): Consider this if your family has a history of cardiovascular diseases, which often correlate with hypertension.
Personal Health Factors Assessment
- Age Factor (5 points): If you’re above 35 years old, the risk of hypertension typically increases, so add points accordingly.
- High-Risk Ethnic Group (10 points): Certain ethnic groups, like African Americans, are at a higher risk for hypertension. If you belong to a high-risk group, assign points.
- Existing Health Conditions (10 points): If you have conditions like diabetes, obesity, or kidney disease, these can contribute to increased blood pressure.
Lifestyle Factors Analysis
- High Sodium Diet (5 points): A diet rich in salt can elevate blood pressure. If your diet is high in sodium, add points.
- Low Physical Activity (5 points): Sedentary lifestyle is a risk factor for hypertension. Add points if you have minimal physical activity in your routine.
- Chronic Stress (5 points): Ongoing stress without effective management strategies can impact blood pressure. Assign points if this applies to you.
Scoring Criteria
- 0-10 Points: Lower Genetic Risk
This range suggests a lower genetic risk. However, continue monitoring your blood pressure and maintain healthy lifestyle choices.
- 11-25 Points: Moderate Genetic Risk
A score in this range indicates a moderate risk. Consider implementing lifestyle changes and seek regular medical advice for monitoring.
- 26+ Points: Higher Genetic Risk
Scores in this range suggest a higher genetic risk. Proactive health management, including regular medical consultations and lifestyle modifications, is highly recommended.
Seek personalized advice from healthcare professionals.
Final Thoughts
Managing and preventing hypertension is a complex task that intertwines genetic factors with lifestyle choices. Understanding genetic predispositions provides crucial context, but it’s the daily lifestyle decisions and proactive health management that ultimately determine one’s health trajectory.
Staying informed, engaged, and active in managing personal health is the cornerstone of effectively dealing with the challenges of hypertension, paving the way for a healthier life.
Frequently Asked Questions (FAQs)
Genetics can significantly influence the development of high blood pressure, but it’s not the sole factor. While it’s estimated that 30-50% of hypertension risk is attributable to genetics, lifestyle and environmental factors also play pivotal roles.
Yes, even with a genetic predisposition, you can take steps to mitigate your risk. Maintaining a healthy weight, consuming a balanced diet low in sodium, engaging in regular physical activity, and avoiding tobacco use can all help in preventing hypertension.
Genetic testing can provide insight into your predisposition for hypertension but isn’t typically necessary for its diagnosis or management. Most doctors recommend lifestyle changes and medication based on your blood pressure readings and overall health rather than genetic testing results.
Not necessarily. While having parents with hypertension increases your risk, it doesn’t guarantee that you’ll develop the condition. It’s important to focus on controllable factors, like diet and exercise, to maintain healthy blood pressure.




